On Safety in Engineering Embryos: Engage the Brakes
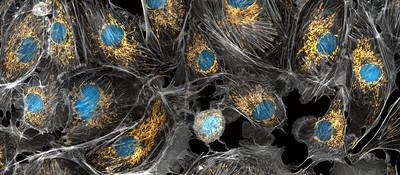
"Golden mitochondria" by National Institutes of Health
(NIH) is licensed under CC BY-NC 2.0.
A controversial embryo engineering technique turns out not to work as planned. It is touted as a way to prevent the births of children with mitochondrial disease, and a few fertility clinics have been using it - without much evidence - to try to circumvent certain varieties of infertility. New information suggests that in the case of preventing mitochondrial disease, the procedure would fail at least 20% of the time, possibly much more.
The technique is variously known as “mitochondrial transfer,” “three-person IVF,” and “nuclear genome transfer” (the most technically accurate). It involves cellular engineering of embryos, rather than changes to DNA. But the revelation of its frequent failure is yet another reason to oppose experiments with heritable genome modification.
Mitochondria are essential for living cells, and their genetic material, known as mtDNA, is separate from what we normally think of as DNA, but both kinds are heritable and both can have disease-causing variations. If a woman has “bad” mtDNA, the idea is to use healthy mtDNA from a donor and combine it with her regular DNA. (That is a somewhat misleading simplification but it conveys the general idea.) Several laboratories are known to be working on developing the technique, but there has been little news of scientific progress. Then Fertility and Sterility published a paper in February with 26 co-authors, including Dagan Wells and Shoukhrat Mitalipov, titled:
First pilot study of maternal spindle transfer for the treatment of repeated in vitro fertilization failures in couples with idiopathic infertility
It reported on six children, each of whom had DNA from both parents (and not from the oocyte donor). Five had mtDNA “almost exclusively (>99%) from the donor.” But one demonstrated surprising changes: As a blastocyst, the mtDNA was 99.2% from the donor, but by the time the baby was born maternal mtDNA constituted 30–60% of the total. This surprising change is known as reversion, and is clearly a concern with as yet unpredictable consequences.
At first, the paper drew little attention, until on March 2nd, MIT Technology Review published an article by Jessica Hamzelou that should be essential reading for anyone interested in heritable genome editing:
Three-parent baby technique could create babies at risk of severe disease
The approach was designed to prevent mitochondrial disease, but new evidence shows it might not work as planned.
In addition to the report in Fertility and Sterility, Hamzelou discovered a presentation, not formally published, which shows that in at least two cases something very strange happened:
In both cases, the proportion of mitochondrial genes from the child’s mother has increased over time, from less than 1% in both embryos to around 50% in one baby and 72% in another.
These results are bad enough to provoke reconsideration of the use of this technology for mitochondrial diseases. Several scientists are quoted in the article as backing away from it, and even the perennially confident Mitalipov admits that at present they have no clue how to solve this problem.
There obviously is an enormous amount we still do not know about heritable genetic alterations. Shouldn’t that give pause not just to mtDNA treatments but to all alterations of DNA in sperm, eggs or embryos?



